|
What causes atrial fibrillation?
There are many risk factors for developing atrial fibrillation, including: increased age, co ronary heart disease, hypertension, congestive heart failure, heart valve diseases or pericardial diseases.
Other conditions that may trigger AF include: chronic pulmonary diseases (pneumonia, asthma, chronic obstructive pulmonary diseases), sleep apnea, previous cardiothoracic surgery, an overactive thyroid gland (hyperthyroidism), obesity, diabetes mellitus, obesity, severe infections, e xcessive intake of alcohol (alcoholism), drinking a lot of caffeine (tea, coffee, etc) and stimulant drug use. However, in up to 15% of patients AF there is no apparent cause for AF and the patient presents a healthy heart. This is called lone AF.
Types of atrial fibrillation
There are several types of atrial fibrillation:
a) Paroxysmal, when the episodes appear suddenly and end spontaneously (without treatment) within 48 hours. The period of time between each episode (each paroxysm) varies greatly from case to case. Although paroxysmal AF stops spontaneously, some people with paroxysmal AF are recommended to take treatment as soon as the AF develops, to stop it as quickly as possible and to avoid that AF becomes persistent.
b) Persistent. This means that AF lasts more than 7 days and it is unlikely to self-terminate, being necessary pharmacological or electrical cardioversion to restore sinus rhythm. However, persistent AF tends to recur, so it may reappear at some point after successful cardioversion.
c) Permanent. This means that AF persists for a long time (= 1 year), just because the cardioversion was unsuccessful or it has not been performed.
What patients may have atrial fibrillation?
Some patients who follow a healthy lifestyle and have no known cardiovascular disease may develop AF. In fact, up to 15% of patients with AF may have a normal heart. In this case we speak of idiopathic AF, i.e., we don´t know the cause of the AF.
In most cases, however, the AF appears in patients with other diseases or risk factors. C oncomitant medical conditions have an additive effect on the perpetuation of AF by promoting a substrate that maintains AF. Conditions associated with AF are:
- Ageing. In fact, the FA appears in the 0.6 % in people over 45 years, 6% in those aged 65 years and over 10 % of people over 70 years.
- Diabetes
- Cardiovascular diseases:
- High blood pressure
- Coronary artery disease (ischemic heart disease)
- H eart failure
- Cardiomyopathies, i.e. diseases of the cardiac muscle
- Valvular heart diseases
- After cardiothoracic surgery
- Hyperthyroidism (over thyroid dysfunction)=
- Chronic obstructive pulmonary disease
- Sleep Apnea
- Obesity
- Chronic kidney disease
- Abuse of alcohol or stimulants
- Serious diseases or infections
What are the symptoms in a patient with atrial fibrillation?
Symptoms are highly variable. In fact, up to 30% of the episodes may be asymptomatic and, therefore, the patient don´t know that he present the arrhythmia. In this case, AF is diagnosed by chance in a routine medical examination of the patient. On the contrary, sometimes the symptoms are quite evident and the patient can recognize the onset of the arrhythmia
Symptoms of AF include:
- Feeling tired or lack energy to perform everyday activities
- Pulse is faster than normal or alternating between fast and slow
- Shortness of breath
- Palpitations (the sensation of skkiping a heart beat or that the heart is running away)
- Difficulty to perform exercise or daily activities
- Pain, pressure, tightness or discomfort in the chest
- Dizziness (feeling light-headed, weak or unsteady), lightheadedness (feeling like you might faint) or fainting
- Increased urination (going to the bathroom more often)
All these symptoms diminish to a greater or lesser degree the quality of life of the patients, so that it is difficult for him to carry out their daily activities.
What complications are associated with atrial fibrillation?
In general, AF is not a high-risk arrhythmia that may endanger the patient's life. However, when the atria"fibrillate"they did not contract effectively, and blood stagnates inside, which favors the formation of clots in the atrial cavities. If the clot breaks off the heart and goes into the bloodstream it results in the formation of thrombi that can block the lumen of a vessel, which prevents the flow of oxygen and nutrients to a specific organ or tissue of the body.
If this happens in the brain a certain section does not receive blood and oxygen, leading to a brain damage which we call stroke. In fact, atrial fibrillation is the cause of approximately 15% of all strokes. The risk of stroke caused by AF increases with age (from 1.5% in patients between 50 and 59 years to 23.5 % in those over 80 years) and the presence of other risk factors such as, for example, heart disease (including diseases of the heart valves, which can increase the risk up to 5 times), high blood pressure and a dilated or enlarged heart.
When the arrhythmia persists for more than 48 hours, the risk of stroke increases, regardless of whether the arrhythmia causes or not symptoms. To avoid these problems, it is necessary to treat all patients with AF of more than 48 hours (or whose duration is unknown) with drugs that prevent the formation of thrombi in the atrial cavities, the so-called anticoagulants (because they prevent clotting) and antiaggreggants (because prevent that platelets bind together and form a thrombus).
Diagnosis
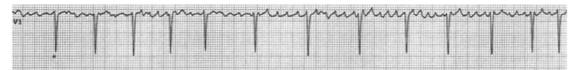
AF is diagnosed with an electrocardiogram (ECG). When the AF comes and goes (paroxysmal AF) and the routine ECG cannot show the arrhythmia it is possible to perform a 24-hour ECG recording (Holter monitoring).
In order to identify the underlying cause of AF it is often necessary to perform blood tests (i.e., to identify an overactive thyroid gland) and an echocardiogram to identify a structural heart problem.
Holter monitor. This a portable ambulatory electrocardiography device for the continuous monitoring of the electrical activity of the heart (electrocardiogram) for at least 24 hours (often for two weeks at a time). Adhesive electrodes are placed on the patient's chest and then connected to a small recorded that is generally placed around the waist. The device contains the hardware (called monitor or recorder) for recording the electrical signals of the heart and software for review and analysis of the record. The Holter is use d in patients with suspected or diagnosed cardiac arrhythmias.
Monitor of events. This is a portable electrocardiogram used in patients who feel an irregular heartbeat occasionally. You take the monitor with you at all times and put it on your chest when you feel the symptoms. This allows the doctor to check your heart rate at the time you have symptoms. This is a very useful device in patients who are asymptomatic.
Echocardiogram. is a noninvasive diagnostic tool that uses high frequency sound waves (ultrasound frequency 2-7 mHz) to obtain accurate pictures of the heart muscle, heart chambers, and structures within the heart such as the valves. A probe connected by a wire to the ultrasound machine and monitor is placed on your chest. To provide good contract between the probe with the skin lubricating jelly is put on your chest. Pulses of ultrasound are sent from the probe through the skin towards your heart. The ultrasound waves then echo ('bounce back') from the heart and various structures in the heart.
Electrocardiogram (ECG). is a simple, painless test that records the electrical activity of the heart to diagnose and assess the risk of any arrhythmia. Small adhesive electrodes are placed on the chest, arms and legs and wires from the electrodes are connected to the ECG machine. The machine detects and amplifies the electrical impulses that occur at each heartbeat and records them on to a paper or computer. A n ECG can help to find the cause of symptoms such as palpitations or chest pain.
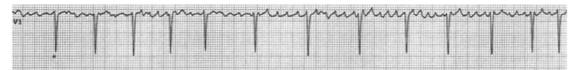
Atrial fibrillation. A characteristic finding that because the atria is firing so rapidly (more than 350 beats per minute) there are no obvious P waves, but the baseline appears chaotic. N ote that the distances/intervals between successive QRS waves (the tall spikes) are irregular in AF due to irregular conduction of impulses to the ventricles.
What is the treatment of atrial fibrillation?
The treatment of AF includes three main strategies that are not mutually exclusive; indeed, in many patients they are used simultaneously:
- To restore and maintain the sinus rhythm and prevent the future recurrences of the arrhythmia (rhythm control). To restore AF to a normal regular rhythm (cardioversion) we can apply to your heart an electric shock or to use antiarrhythmic drug (amiodarone, flecainide, propefenone, vernakalant). The cardioversion is more likely to be considered if your AF developed recently, you are younger than 65, when the underlying cause of the AF has been successfully treated and there are no structural heart diseases. However, cardioversion is usually not an option in patients with long-term AF (usually for more than 12 months), in patients with a structural problem to the heart or when previous attempts of cardioversion have not worked (or only worked for a short time before the heart reverted back to AF). A new technique to restore the heart rhythm is called catheter ablation. In this procedure, the tip of a catheter located into the chambers of the heart can destroy small sections of heart tissue that may be the source or trigger of the abnormal electrical impulses.
To maintain the sinus rhythm, several antiarrhythmic drugs can be used (in alphabetic order): amiodarone, dronedarone, flecainide, propafenone, sotalol.
- When AF can't be converted to a normal heart rhythm, the goal is to slow the heart rate to between 60 and 100 bpm (rate control). Heart rate control can be achieved with some antiarrhythmic agents that slow the conduction through the AV node (amiodarone, beta-blockers, digoxin, diltiazem, verapamil). The aim of treatment is to bring the heart rate back down to normal (ideally, to less than 90 beats per minute when resting).
- To prevent thromboembolic events using anticoagulant agents that reduce the chance of forming a blood clot and having a stroke and antiplatelet agents that inhibit platelet aggregation. For the past six decades vitamin K antagonists (acenocumarol, warfarin) have been the only agents used for long-term oral anticoagulant therapy. Recently, newer anticoagulants for the prevention of thromboembolic or ischemic events appeared, including direct thrombin inhibitors (Dabigatran) and d irect factor Xa inhibitors (Apixaban, Rivaroxaban). The main adverse effect of the these drugs is that they increase the risk of bleeding. Warfarin can interact with many different drugs, foods and herbal medicines. However, up to now the new oral anticoagulants, such as dabigatran, apixaban and rivaroxaban, do not present these interactions.
If you take warfarin you will need regular blood tests (INR tests) to get the dose of warfarin that you need, so your blood does not clot as easily as normal, but not so much as to cause bleeding problems. Blood tests may be needed quite often at first in order to know the best dosing regimen, but often frequent afterwards. Dabigatran, apixaban and rivaroxaban do not need regular blood tests.
Aspirin is a platelet antiaggregant that has been used in the past; however, aspirin is not as effective as warfarin. Thus, it is nor recommended for clot prevention in AF.
- In addition, it is recommended that strict control of those diseases that are frequently associated with AF, such as hypertension, heart failure, ischemic heart disease, diabetes or hyperthyroidism.
|